Get your digital files instantly after purchase
Nursing Soap Note
$2.50
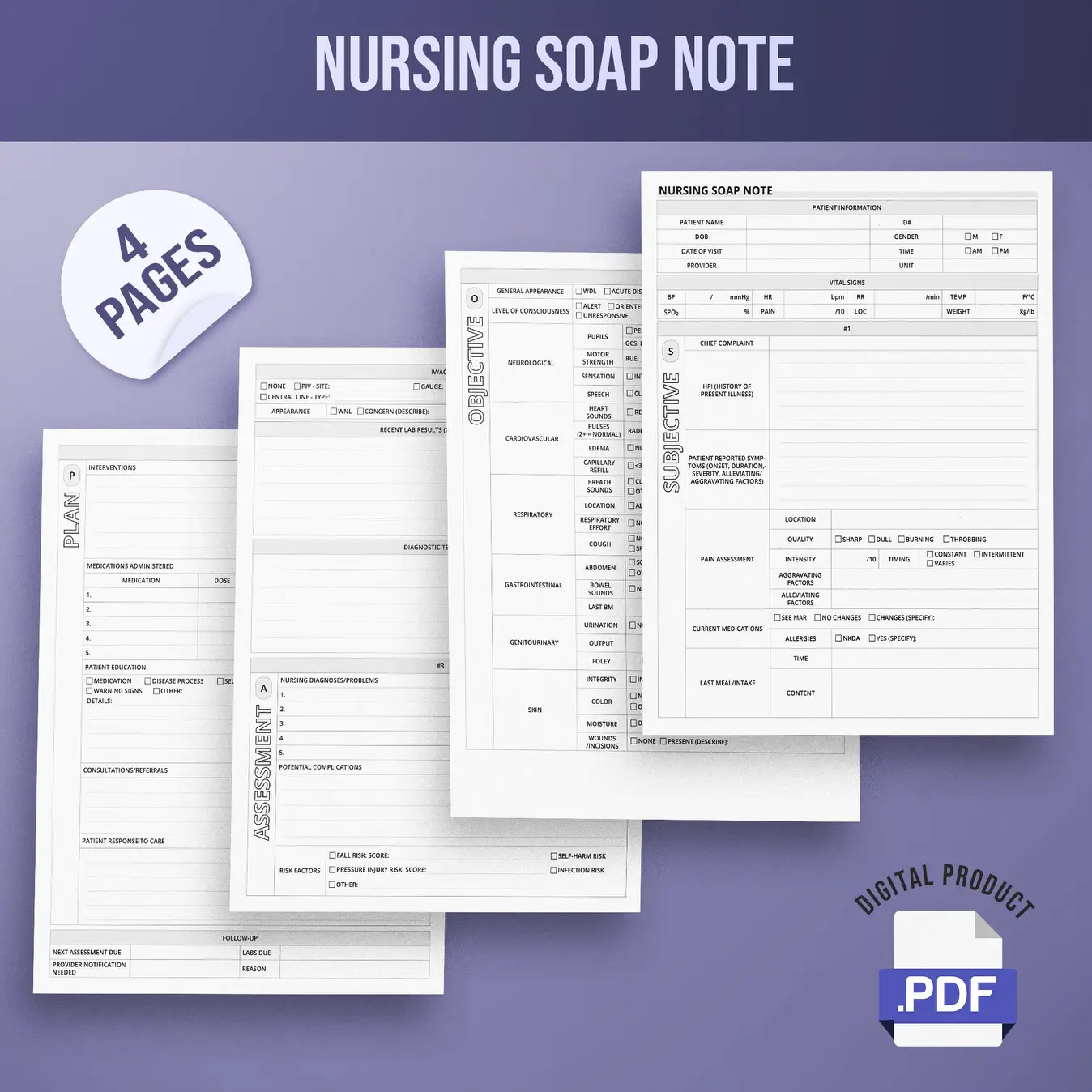
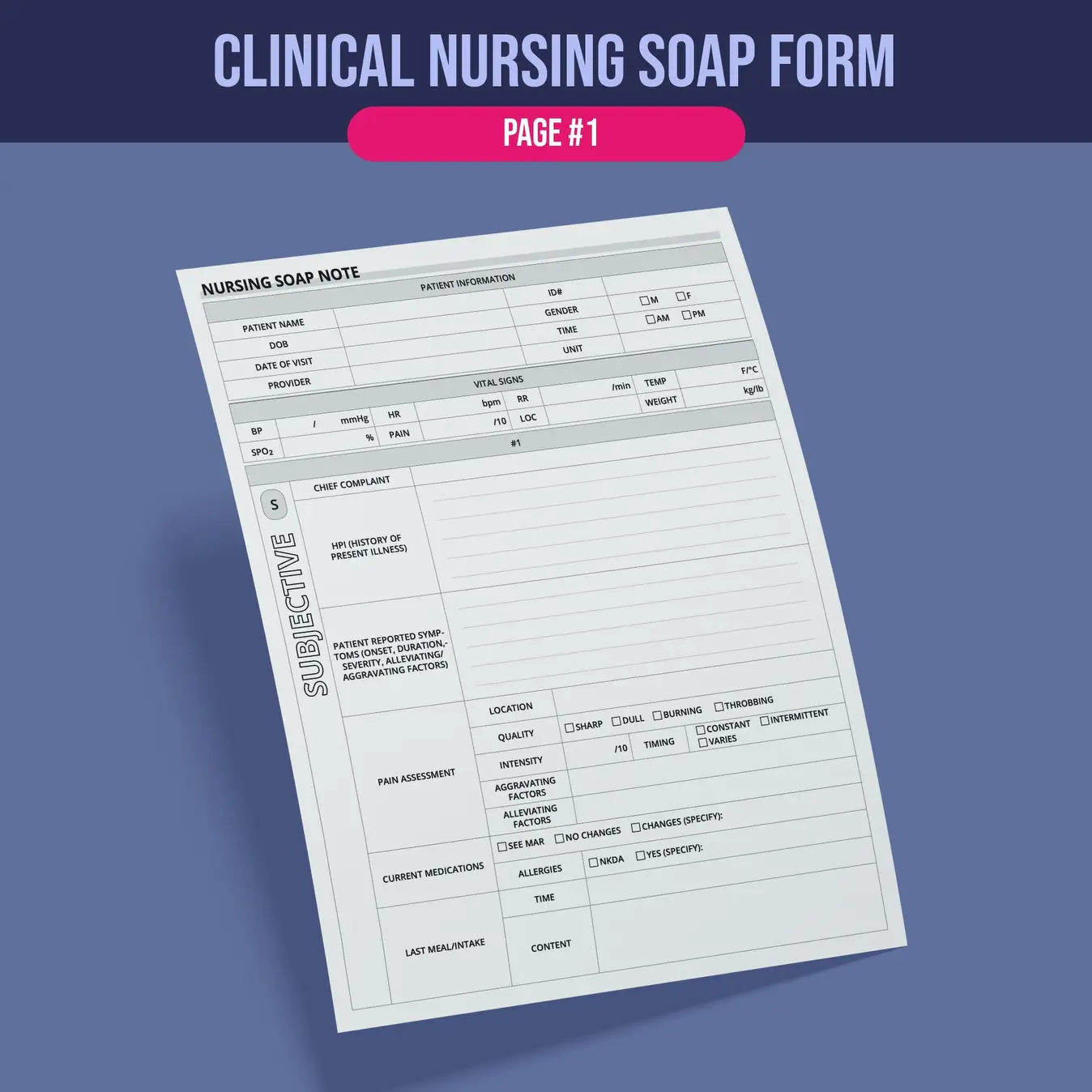
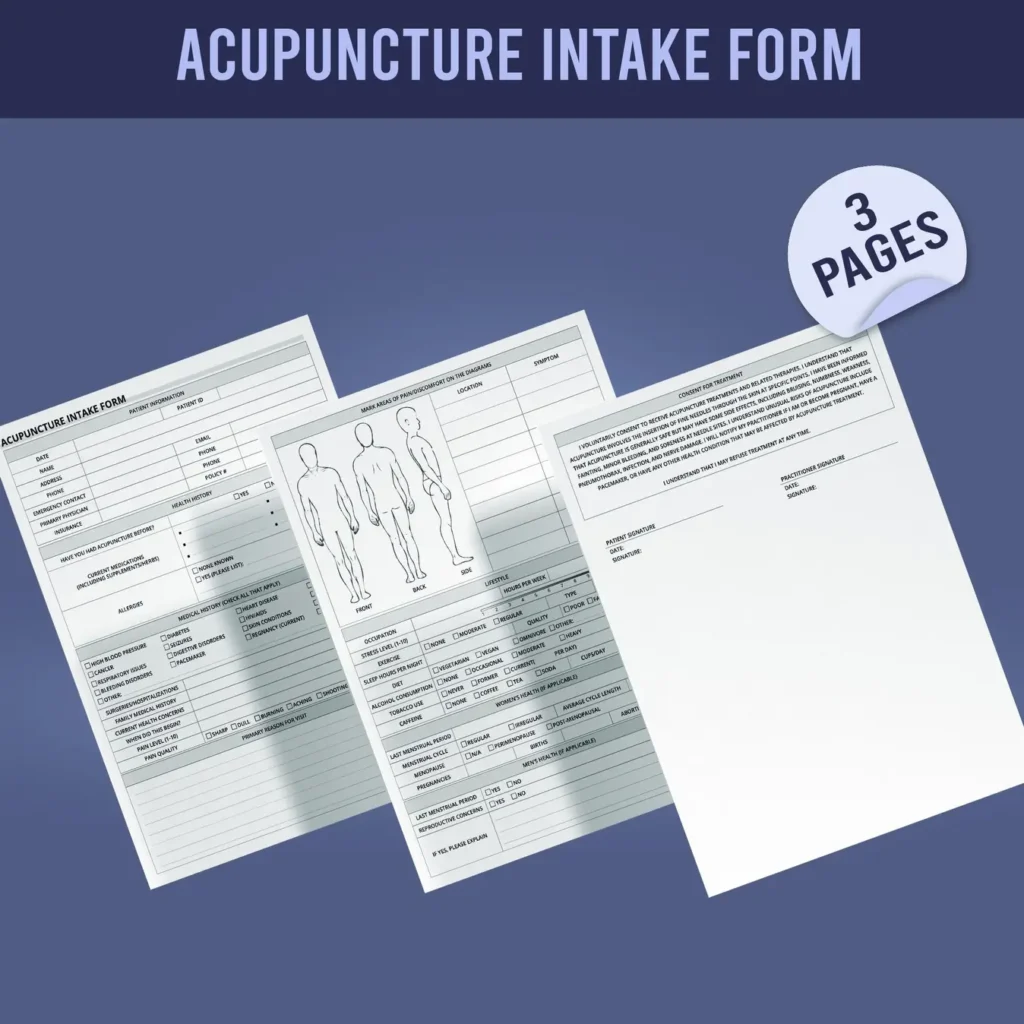
Professional SOAP note template for nurses—systematically document patient encounters with sections for subjective, objective, assessment, and plan. Perfect for clinical documentation.
Specification
Overview
 Number of Pages
Number of Pages
|
04 Pages |
|---|---|
 File Type(s)
File Type(s)
|
|
 Dimensions
Dimensions
|
US letter (8.5 x 11 in) |
 Language
Language
|
English |
 Delivery Method
Delivery Method
|
Instant Digital Download — No physical item will be shipped |
 Usage
Usage
|
Unlimited prints allowed |
Description
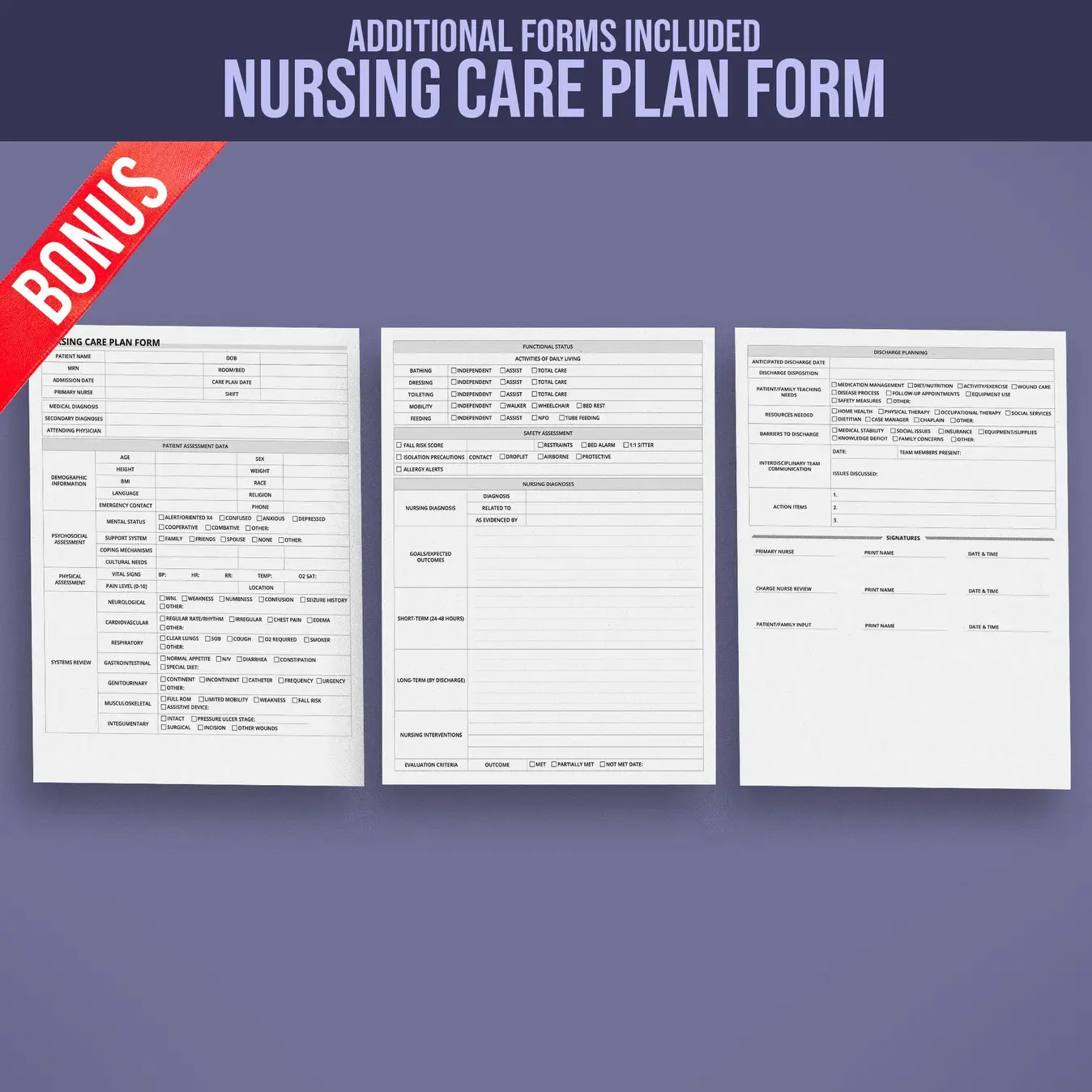
Enhance your nursing documentation with this structured SOAP Note template, designed to streamline patient record-keeping using the proven SOAP methodology for comprehensive care coordination.
- Patient Information – Name, age, gender, and relevant medical history
- Subjective (S) – Patient’s reported symptoms, concerns, and history
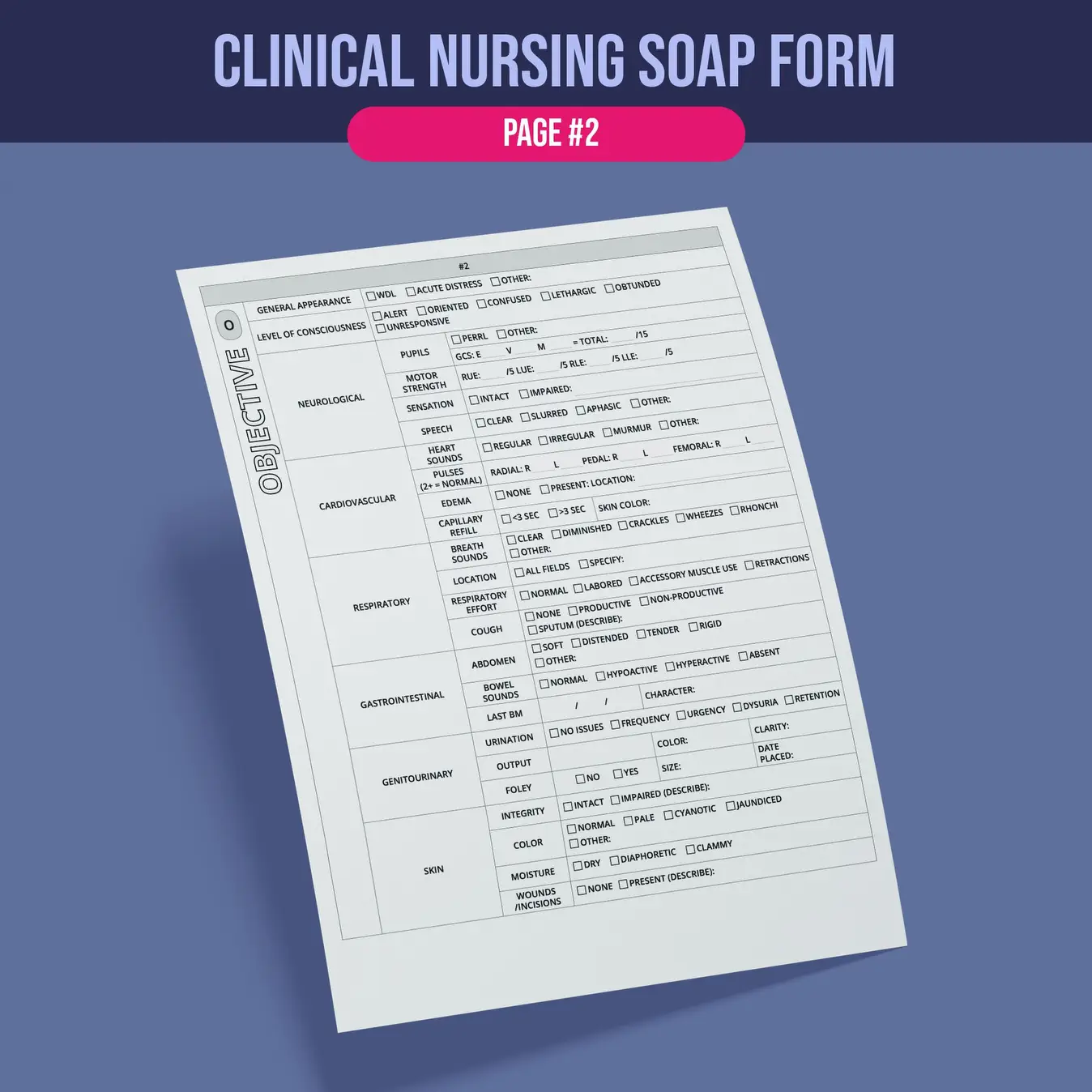
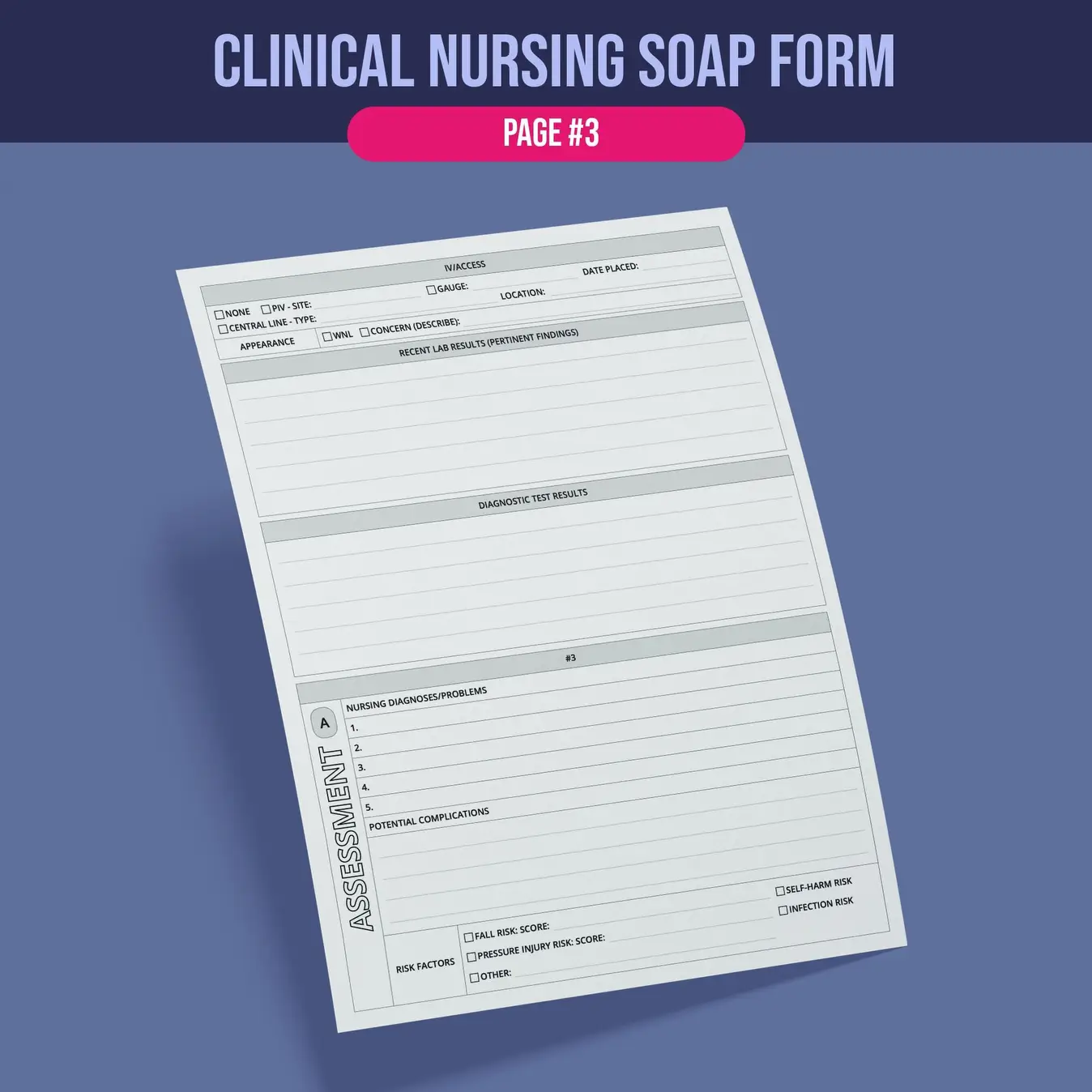
- Objective (O) – Measurable data: vitals, exam findings, test results
- Assessment (A) – Clinical interpretation and diagnosis
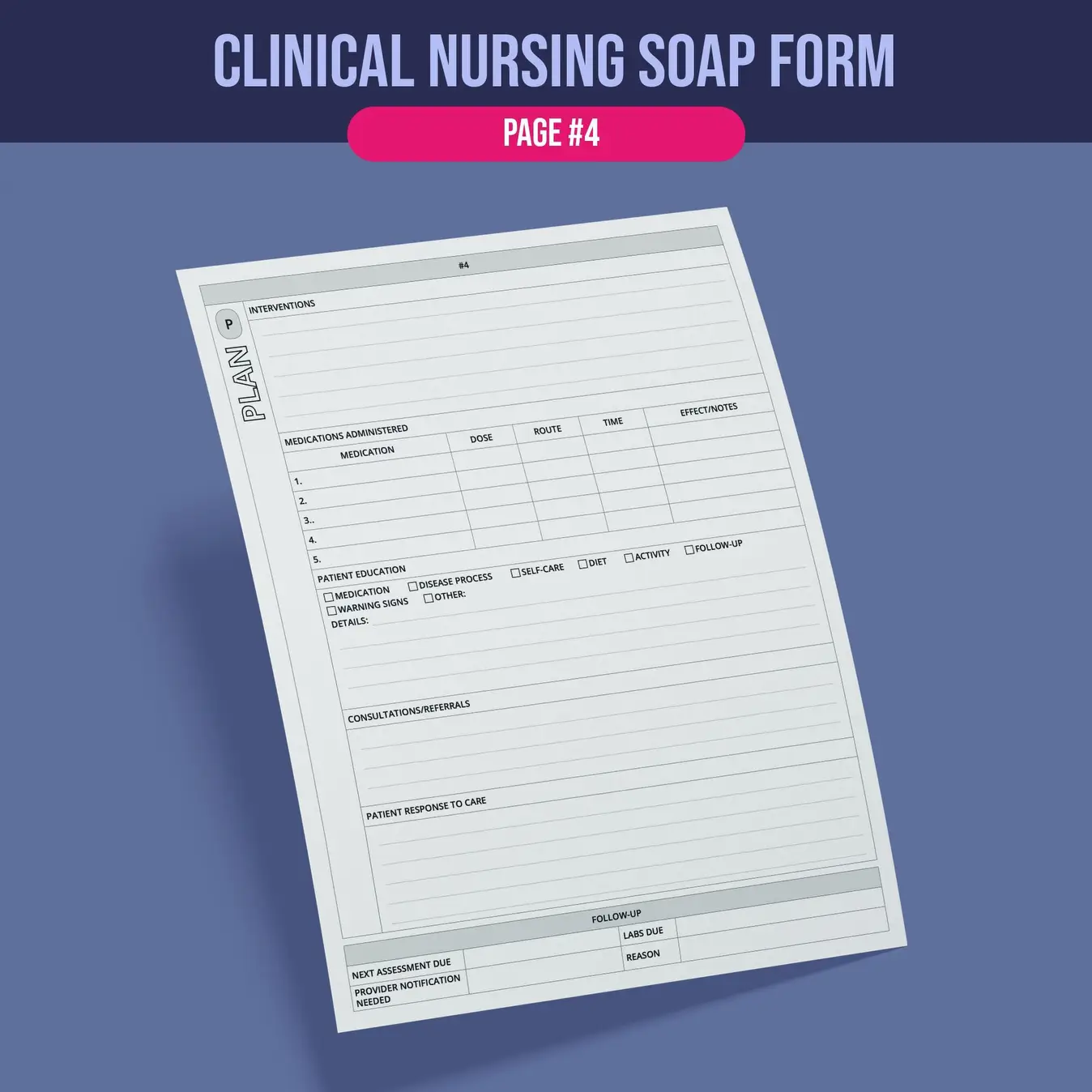
- Plan (P) – Treatment strategy, medications, and follow-up
Ideal for RNs, nurse practitioners, and nursing students in hospitals, clinics, or home healthcare settings who need efficient, standardized documentation that improves care continuity and meets compliance requirements.
Customer Reviews
Samantha R.
Super easy to download and print. The layout is clear and very useful for my daily tasks!
Mark T.
Exactly what I needed! Saved me time and looks professional. Will definitely purchase more from this shop.
Elena G.
Simple, clean design and very well-organized. I use it weekly and it’s made my life easier.
Jordan P.
I love how convenient this is. Great value for the price and super helpful for staying on track.
Ava L.
The design is great and it printed nicely, but I wish there were more layout options included. Still happy overall!
Caleb M.
The files were delivered instantly and everything was just as described. Highly recommend this shop!